A Practical Guide to Using Consensus Methods in Integrated Evidence Planning
Consensus methods provide Medical Affairs teams with a practical, scientifically rigorous approach to bridging evidence gaps that clinical trials and real-world studies alone may not fully address. By systematically capturing and synthesizing expert insights, these methods can help establish best practices, shape treatment algorithms, and align both internal strategies and external stakeholder engagement.
Success, however, depends on execution. From defining the right use case and selecting the appropriate methodology to assembling a credible expert panel and embedding the findings within the broader evidence and communication plan – every step plays a critical role in integrated evidence planning. This article offers a clear, step-by-step framework for designing, executing, and maximizing the impact of consensus studies.
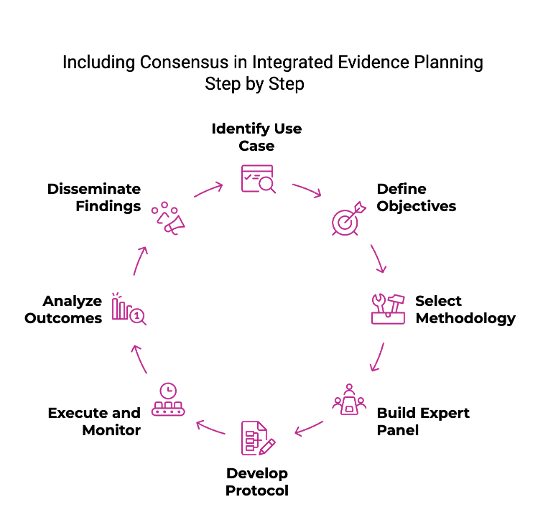
Step 1: Identify the Right Use Case
The first step begins with a comprehensive mapping of existing and planned data across the product lifecycle. Clinical trials, real-world evidence studies, HEOR analyses, and investigator-initiated trials may all address certain questions, but gaps inevitably remain.
The decision to initiate a consensus study should be grounded in both clinical need and business relevance. Diagnostic uncertainty, variation in care standards, and inconsistency in treatment outcomes are all strong indicators that a consensus approach could be beneficial.
Engagement with field medical teams, regional medical directors, and external stakeholders early on can help validate the use case and ensure that the study addresses meaningful and timely questions.
Step 2: Define Clear Objectives
Objectives should be specific, measurable, and aligned with broader evidence and communication strategies. Examples might include defining when to initiate therapy with a newly approved agent, agreeing on a diagnostic algorithm for a rare condition, or establishing consensus around relevant clinical or patient-reported outcomes for future studies.
Importantly, objectives should be designed not only to generate publishable insights but also to produce practical outputs such as clinical decision tools, treatment algorithms, or value narratives that can be used by external stakeholders. This dual focus on academic and applied utility enhances the long-term impact of the consensus study.
Step 3: Select the Appropriate Methodology
Selecting the right methodological framework is critical to ensuring that the process of achieving consensus is both scientifically valid and operationally feasible. The choice of method should reflect the complexity of the topic, the degree of consensus needed, and the time and resource constraints of the Medical Affairs team.
Delphi panels are ideal for situations that require anonymous, iterative feedback from a geographically dispersed panel. It allows for refinement of opinions over multiple rounds and reduces the influence of dominant personalities. The Nominal Group Technique (NGT), in contrast, is better suited to highly interactive, structured discussions where consensus is built through group dialogue and immediate ranking of ideas. The RAND/UCLA Appropriateness Method is particularly effective when the goal is to evaluate the clinical appropriateness of specific interventions, combining evidence review with expert scoring.
Step 4: Build the Expert Panel Thoughtfully
The credibility of a consensus study hinges on the expertise and diversity of its panel. Medical Affairs must ensure that panel members are not only leaders in their respective fields but also represent a range of practice settings, geographic regions, and clinical perspectives.
Including a mix of academic thought leaders, community-based clinicians, and cross-specialty experts (when appropriate) enhances the robustness and applicability of the study’s findings. Additionally, involving emerging voices such as younger clinicians or those from underrepresented health systems can bring fresh insight and reflect real-world practice more accurately.
Panel selection should be grounded in transparent criteria and conducted in alignment with compliance and transparency guidelines.
Step 5: Develop a Rigorous Protocol
Consensus studies must follow a scientifically rigorous and transparent process. A well-developed protocol serves as the backbone of the study and should include clearly defined research questions, objectives, rationale for the chosen methodology, and criteria for achieving consensus.
Defining what constitutes consensus is particularly important, this may involve a predefined percentage agreement (e.g., 75% consensus threshold) or statistical metrics such as interquartile ranges, depending on the methodology. The protocol should also describe how responses will be collected, analyzed, and validated.
Step 6: Execute and Monitor with Precision
Execution of a consensus study requires careful project management and scientific oversight. Timelines must balance efficiency with the iterative nature of the process, particularly in Delphi studies where multiple rounds of feedback are involved. Leveraging validated platforms for survey distribution or virtual discussion can improve response rates and data integrity.
Anonymity is critical in some methods (such as Delphi panels) to minimize bias and allow participants to express their views freely. In other methods, fostering real-time interaction and debate may be more productive.
Ongoing communication with panel members and timely reminders can help keep the study on track, while periodic check-ins with internal stakeholders ensure alignment with broader strategic objectives.
Step 7: Analyze, Validate, and Document Outcomes
It is essential to analyze the data using appropriate qualitative or quantitative techniques. For structured surveys, this may involve calculating agreement levels, identifying patterns of divergence, and presenting results visually (e.g., heatmaps or consensus matrices). For discussion-based studies, thematic analysis can uncover recurring concepts and consensus points.
Validation is an equally important part of this phase. Results should be reviewed by an internal scientific committee or an external steering group to confirm the integrity and relevance of findings. This validation ensures that the conclusions drawn are not only methodologically sound but also clinically meaningful.
Step 8: Disseminate Strategically
The final step is dissemination, making sure that the consensus findings are shared with the right audiences, at the right time, through the right channels. Peer-reviewed publication remains the gold standard for credibility and reach, but should be complemented by other activities for broader visibility.
Internally, the insights can support field medical training, inform scientific messaging, and enhance HEOR models or access dossiers. For example, a treatment algorithm derived from a consensus panel can become part of a payer value story or a clinical decision-support tool deployed by MSLs.
Importantly, dissemination should be integrated into the evidence plan from the outset. Aligning consensus outputs with strategic objectives, from data-to-communication, ensures that they are not just informative but fostering real change.
Conclusion
Consensus methods are a powerful way for Medical Affairs to address evidence gaps and drive meaningful insights. When executed thoughtfully, they deliver actionable outputs that support clinical practice, stakeholder engagement, and strategic objectives. By following a structured approach, teams can ensure these studies are both scientifically sound and impactful.
About us
At Triducive we deliver consensus-led evidence that gets published and supports change, collaborating with medical affairs and other teams in life sciences all around the world. With a strong background in healthcare, we have been delivering 130+ Delphi consensus to date, helping to change practice and guidelines, improve pathways, and support payers’ decisions.
Get in touch with us to learn about how a consensus study can help you achieve your objectives.

